Movement Matters in Children with Autism

Kunali Doshi
DHA License Number: 00100771-002
Senior Pediatric Physical Therapist
Introduction
Autism Spectrum Disorder (ASD) is a developmental disability characterized by persistent impairments in social communication and the presence of restricted repetitive patterns of behaviours, interests, or activities, sensory processing challenges, and a differently wired brain with diverse gifts and talents (Kim Barthel, 2020).
The past few decades have shown increasing incidence of ASD with one in every 36 eight-year-old children have been identified with ASD, according to an analysis published in CDC’s Morbidity and Mortality Weekly Report in 2023 (www.cdc.gov/ActEarly).
ASD symptoms might be detected within the first 12 months of age. In others, symptoms may not show up until 24 months of age or later. Some children with ASD gain new skills and meet developmental milestones until around 18 to 24 months of age, and then they stop gaining new skills or lose the skills they once had.
The wide spectrum of autism has changed our manner of treating a diagnosis from “a one-size fits all” approach to a holistic one that recognizes the fact that there are multiple complex needs. This way, we bring compassion into our treatment and tap into the core values of every human being no matter what their differences are. Current ASD treatments seek to reduce symptoms that interfere with daily functioning and quality of life. Treatment plans usually involve multiple professionals and are catered to the individual. Traditionally, Autism is presumed to be synonymous with behavioural, sensory, and perceptual abnormalities. However, a recent study revealed that 87% of school-age children with ASD within the United States were at risk for motor impairment and did not change by 15 years of age. (Bhat A, 2020).
Identification and treatment of motor issues in children with ASD is important because the lack of full movement repertoire affects a child’s play and interaction with peers and caregivers, and adds to their social-emotional difficulties.
A lack of inclusion of motor impairments within ASD diagnostic criteria may contribute to a lack of recognition and poor diagnosis and treatment of motor challenges.
General Movements (GMs) are a distinct movement pattern carried out spontaneously without external stimulation and seen in foetuses of 9 weeks gestational age till 21 weeks post term. (Phagava H, et al.2008)
Early Intervention is now considered the core treatment strategy for ASD.
If Autism is more of a social issue, why does it need Physical Therapy (PT)?
While social and behavioural issues are more obvious in children with ASD, some characteristic physical features related to their gross motor function and movement may also be noticed. These may also add to their difficulties in interacting with their environment.
Although only repetitive behaviours are included in the diagnostic criteria, motor impairment is a cardinal feature in ASD (Fournier et al., 2010)
More than increasing our quality of life from a basic survival point of view, movement plays a significant role in our connecting with people and in supporting our physical and emotional health.
Babies and infants communicate through movements. They use non-verbal aids such as movement of facial muscles, movement of hands and feet, and movement of their trunk. These interactions are interpreted by the caregiver which in return forms a bond/relationship with the caregiver. If the baby can’t make these movements and responds differently, it takes the relationship out of sync.
Neuroscience is increasingly showing that movement improves our cognition and ability to learn. Additionally, movement contributes to our interoception (awareness of the body’s sensations from within), awareness of oneself.
Movement is affected by lots of different pieces in a neurodiverse brain, and it brings different parts of the brain together.
One of the first features that help discern or diagnose that a child might have ASD shows up in infancy in the movement system. Atypical motoric function is one of the most frequently reported signs of ASD during early development (Annio Posar and Paola Visconti, 2022).
Some Red flags in the movement system in children with Autism:
- Low muscle tone or floppiness which may be visible in the way the child struggles to come up against gravity to sit, stand or come to all fours. These children may avoid physical activities like running, jumping, and hopping and may experience more frequent falls and clumsiness.
- Asymmetry in posture is noticed as there may be a difference in two sides of the body, patterns of compensations where one arm or leg has to work harder to keep the body still so that the other side can do its job. Difficulty bringing hands together is noticed in infants and babies.
- Orientation: how the child moves the body in relationship to the world is affected. For example, if you call out the child’s name, and the child may not be able to respond by turning their face and leaning towards you. This body orientation helps connecting to objects and people. In children with ASD, you will observe reaching out without looking, odd orienting response, not turning to look and reach for an object.
- Mobility: how does the child move from place to place. The child may be having an increased tone which can cause tip-toe walking, to decreased/low muscle tone and walking either with flattened feet or compensating by going up onto their tiptoes to walk.
- Repetitive action without a purpose.
- Muscle weakness such scapular winging, hyperextension of the knees and reluctance to lift heavy objects.
- Generalized hyper mobility of joints such as flat feet, hyperextension of elbows and knees on passive movement, poor posture, etc.
- Poor eye-hand and eye-foot coordination
- Poor core stability and balance with difficulties in single limb standing that is required for ball kicking.
- Posture and gait deviations such as lordotic posture while standing, kyphotic posture in sitting and protracted shoulders.
- Limb apraxia i.e difficulty performing planned movements of arms or legs. For example, moving body parts to get into a tunnel or climb up
- Poor execution of sequential planning of activities, difficulty in starting or stopping movement on request, imitation, turn taking and following directions.
on a swing.
These behavioural observations are in line with neuroimaging-based findings and histological studies on brains of humans with ASD, in which atypical patterns have been reported regarding the morphology and function of motor-related neural regions, such as basal ganglia and cerebellum (Subramanian K,etal., 2017).
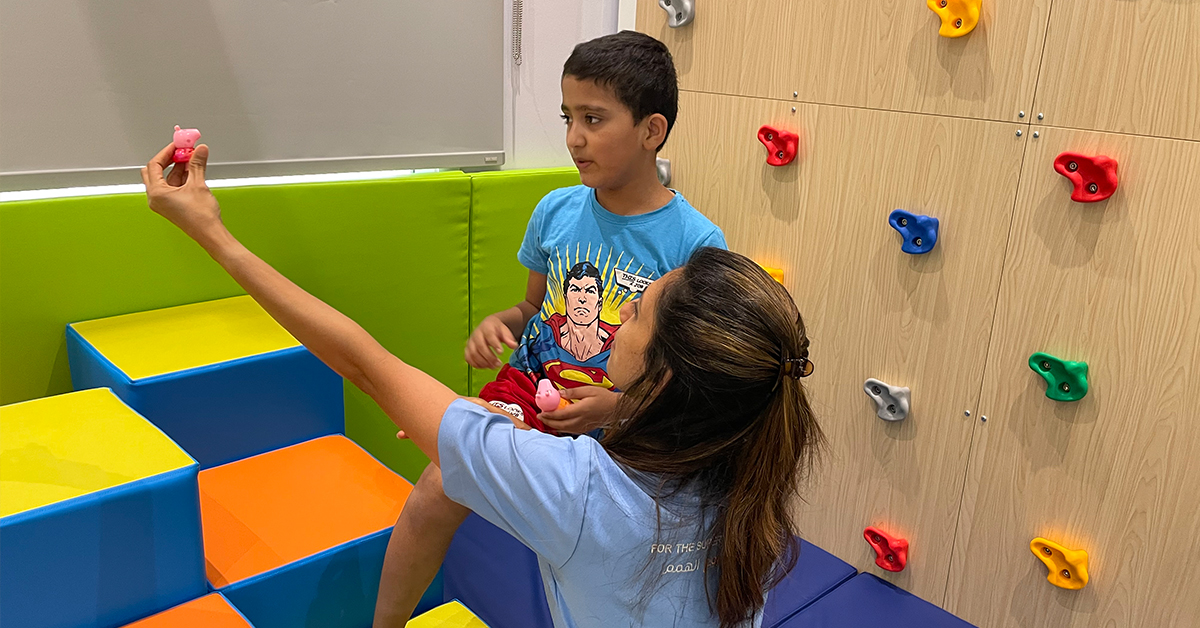
Role of Physical Therapy
Physical therapy brings about functional change in ease of movement, in activity, in arousal and affect, and last but not the least in relationship. It helps the child embody the sensory and motor experience that they have in sessions to be translated in embodied experiences in everyday functions.
The following are some of the movement matters that would be focussed on during PT sessions:
- To achieve their gross motor development such as sitting, rolling over, standing, and walking.
- To improve core strength and overall muscle tone of the body.
- To improve coordination and balance using dynamic surfaces such as a ball, bosu, wobble board and swing.
- To improve the postural muscle tone and enable more efficient limb movements.
- To work on motor planning and execution of movement on request, by imitation and to follow directions using play-based activities.
- To develop reciprocal play skills such as catch and throw, kicking and targeting.
- To incorporate bilateral integration of body parts in movements like jumping.
- To build strength and endurance of these children who will soon be young adults in a long-haul perspective.
Creative interventions such as yoga and hydrotherapy are also promising tools for enhancing motor and coordination skills in children with ASD.
What does Research say?
Research based study recently showed a large correlation between social skills and gross motor skills in children with ASD. Those with higher gross motor skills also had higher social skills. Those with poorer gross motor skills (specifically object manipulation skills) and poor core strength/stability demonstrated the most delays in social and behavioural skills.
A new study in 2018 looked at a 48wk exercise program that improved quality of life, metabolic measurements, and autistic traits in the experimental group of children aged 6-12 years with ASD (Toscano CVA et al., 2017). This study is supporting the role of the physical therapist in promoting physical activity (PA) participation and getting a child with autism involved in community level PA.
The 360-degree Approach is an all-embracing, across-the-board approach that encompasses all the variables that impact the life of the individual with autism and at its core, simply refers to the absolute need for all parties involved in an autistic person’s life to place her, or him, in the centre.
Working hand in hand with a child’s Occupational Therapist and Speech and Language Therapist, a Physical Therapist could incorporate therapeutic goals into a session to treat the child as a whole. We must empower these neurodiverse beings to be responsible for their own bodies in the future (Regie Bane).
Sources:
- Online Course provided by Kim Barthel on Autism Matters in 2021
- Bhat A, Motor Impairment Increases in Children With Autism Spectrum Disorder as a Function of Social Communication, Cognitive and Functional Impairment, Repetitive Behavior Severity, and Comorbid Diagnoses: A SPARK Study Report, Autism Research,2020
- Annio Posar and Paola Visconti , Early Motor Signs in Autism Spectrum Disorder, Children (Basel)2022
- Doi Hirokazu et al. prediction of autistic tendencies at 18 months of age via markerless video analysis of spontaneous body movements in 4-month-old infants Sci Rep 2022
- Toscano CVA , Carvalho HM , Ferreira JP, Percept Mot SkillsExercise Effects for Children With Autism Spectrum Disorder: Metabolic Health, Autistic Traits, and Quality of Life, 2017
- Phagava H, Muratori F, Muratori F, Maestro S, Apicella F, Guzzetta A, Prechtl HF, Cioni G, General movements in infants with autism spectrum disorders, Georgian Med News,2008
- Subramanian K,Brandenburg C, Orsati F, Soghomonian J, Hussman J, Blatt G, Basal ganglia and autism – a translational perspective,Autism Research, 2017