Let’s Talk About… Pathological Demand Avoidance (PDA) in Autism

Alycia Beaman
Speech and Language Therapist
DHA License Number: 93427730-002

Last month, we celebrated Autism Awareness Month—a time to recognise not just autism itself, but also the less commonly known traits and diagnoses that accompany it. One of these is Pathological Demand Avoidance (PDA), a profile seen in some autistic children that is often misunderstood or entirely overlooked.
Understanding PDA: A Different Operating System
Imagine comparing Apple and Android phones. Both make calls and send messages, but the way they operate is completely different. This is similar to how neurodivergent brains, including autistic ones, process the world compared to neurotypical brains. Both are capable—just wired differently (Keeble, 2021).

So, what is PDA?
PDA is not yet a formal diagnosis in the DSM-5 (the manual most professionals use), but it is a very real experience for many families, particularly those with autistic children.
Key Characteristics:
- Avoidance or resistance to everyday demands—even things the child usually enjoys
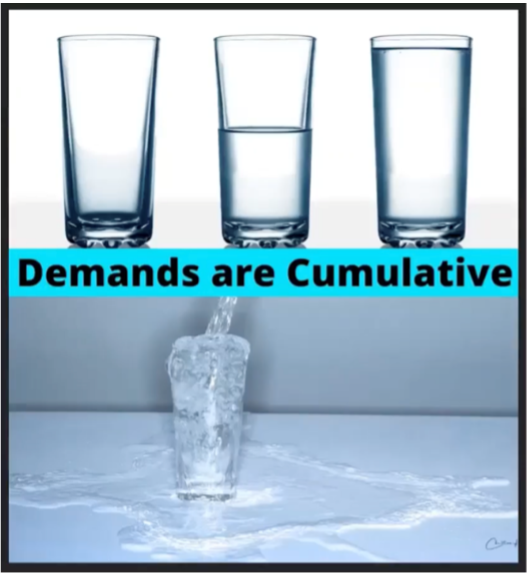
- A survival drive for autonomy that can override other survival needs (e.g. eating, sleeping, hygiene, safety, toileting), either in the moment or cumulatively (leading to burnout)
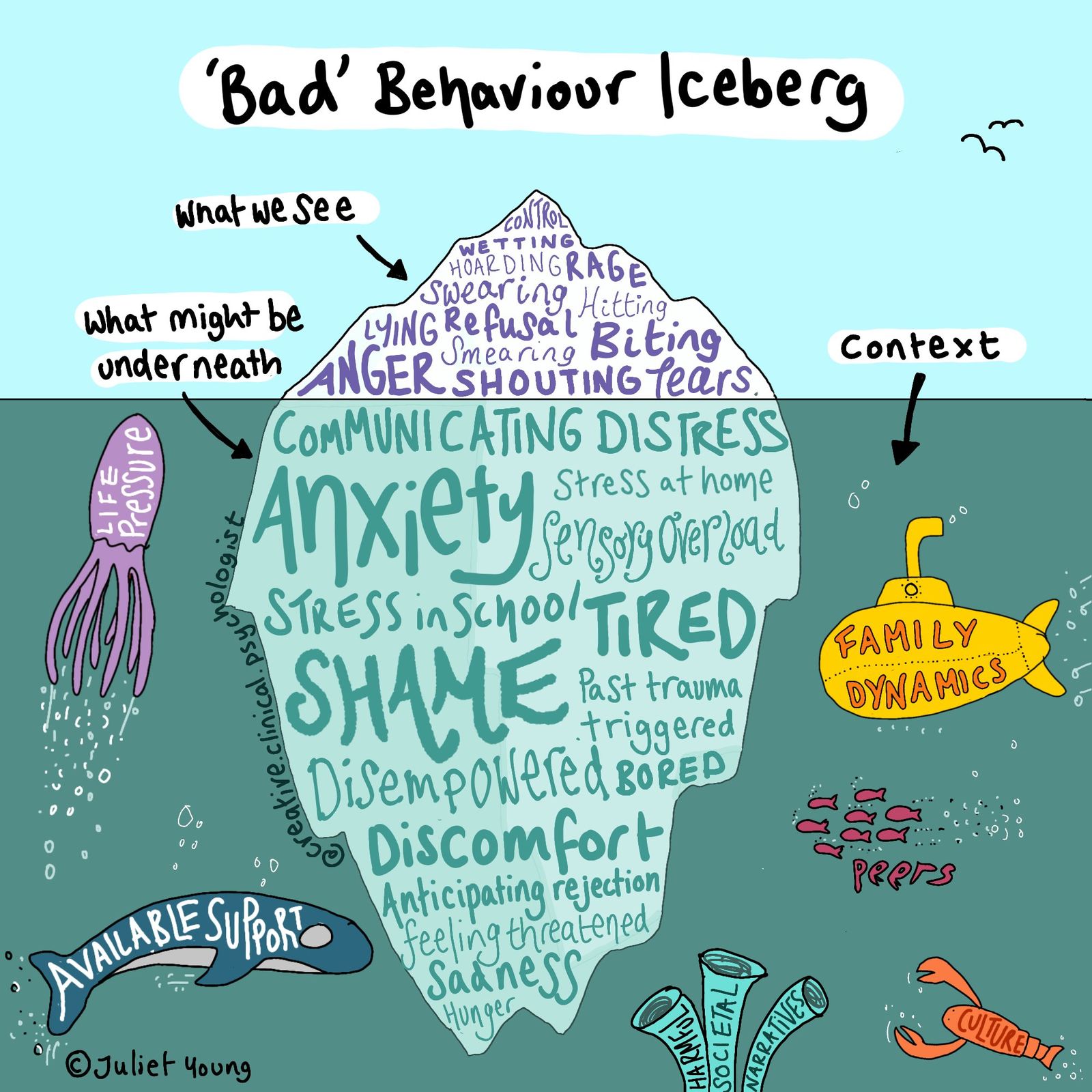
- Controlling or defiant behaviour, often stemming from a fight-or-flight response to perceived pressure
- Seeking connection and comfort through fantasy and imaginative role-play, sometimes to an extreme
- Intense emotions and a need constant emotional support from trusted adults (e.g. nervous system co-regulation)
- Frequent and recurring nervous system activation (fight-or-flight) in response to demands, often recognised when the child reaches burnout
- A strong focus on others, which may show up as social fixations or intense interests in real or fictional people
- Masking difficulties by appearing social or talkative-engaging in reciprocal conversation and eye contact while hiding deeper struggles with social skills. The PDA child or teen often appear like two very different people of depending on the context
Children with PDA are often misdiagnosed with ADHD or Oppositional Defiant Disorder (ODD). Traditional parenting or behaviour plans don’t help and can even contribute to more stress or emotional harm (e.g. complex trauma and nervous system burnout). (Ehrlich, 2022).
What Counts as a “Demand”?
Demands are anything that feels like an expectation. These include:
- Sensory overload, transitions, or even favourite activities and hobbies
- Direct requests like “put on your shoes” (declarative language)
- Questions-responding directly can feel overwhelming
- Internal needs like hunger or needing the toilet
- Praise, which may feel like pressure to repeat success
- Uncertainty-the need to know and feel in control can be extreme
Wait… What is the Difference Between Extreme Anxiety and PDA?
- Extreme anxiety is typically a cognitive process-worrying about future events, which then triggers a fight-flight-freeze or avoidant response
- PDA does not necessarily involve future-based worry. The avoidance often stems from a perceived loss of autonomy or equality, especially when someone (e.g. a caregiver) is seen as trying to “make” them do something. This can trigger a subconscious fight-flight-freeze reaction or complete avoidance
What Can Help?
Children with PDA thrive with understanding, flexibility, and trust—not strict routines, rewards, or punishment. Supportive strategies include:
- Low-arousal approaches focused on recognising and managing underlying anxiety
- Keeping routines predictable, but being flexible with changes
- Supporting sensory needs
- Using visuals or visual stories to prepare for events
- Speaking with calm, non-threatening language (e.g. “I notice that…”, “I can see that…”, “how about we…”)
- Using humour, distraction or role-play to reduce anxiety
- Offering choices and involving the child in decision-making as well as working collaboratively to solve problems
- Giving plenty of notice about any changes within reason or accepting that avoiding some things is perfectly fine
- Establishing clear, safe boundaries in home and school settings
- Building the child’s interoception, self-awareness, self-esteem, resilience, and self-advocacy.
As Dr. Ross Greene says, “Kids do well if they can.” No child chooses to experience crippling anxiety, panic attacks, meltdowns or nervous system burnout.
For Parents
If you’re parenting a child or teen with PDA, you’re not “giving in.” You’re learning a different way to connect. As Dr. Casey Ehrlich reminds us: “You are making space in your brain and heart for a new way of parenting. And that is powerful.”
If you would like to know more about this topic or require professional support for your child dealing with PDA, please contact our speech therapy team at High Hopes.
Sources:
- Keeble, C. J. (2021). [Seminar on neurodiversity and PDA].
- Ehrlich, C. (2022). Parenting strategies for PDA and demand-avoidant behavior.
- Website link – https://www.pdasociety.org.uk/
- Website link – https://www.atpeaceparents.com/
- Greene, R. (2016). The Explosive Child.